
What is Alzheimer’s Disease?
Alzheimer’s disease (AD) is a kind of dementia that typically starts after the age of 65 years and gradually worsens over time. People with Alzheimer’s disease have trouble with learning and memory, word finding, and remembering how to do certain tasks.
Family members often comment on their loved one’s changes in behaviour, such as:
- Repeating questions and statements
- Forgetting to pay bills or take medications
- Problems remembering what time, date, or year it is
- Getting lost in familiar places
- Word-finding difficulties or “word slips”
- Lapses in judgment or problem solving
Often the person with Alzheimer’s disease is not aware of their worsening cognitive problems. Apathy, agitation, or depression is not uncommon. Often, but not always, there is a history of Alzheimer’s or dementia in a first degree relative of the affected individual.
I’m Having Memory Problems – Do I Have Alzheimer’s?
Inefficiencies in short-term memory and trouble “finding our words” are common complaints of normal aging. We also experience memory lapses and foggy thinking when we are under increased life stress, in physical pain, anxious, or feeling depressed. Our neuropsychologists can help diagnose and treat the reasons underlying any cognitive changes.
What Causes Alzheimer’s?
![]() There is no specific known cause of the disease, although a combination of genetic and environmental factors plays a role in the disease. There is no known cure for Alzheimer’s disease. However, there are medications, lifestyle factors, and therapies that may help.
There is no specific known cause of the disease, although a combination of genetic and environmental factors plays a role in the disease. There is no known cure for Alzheimer’s disease. However, there are medications, lifestyle factors, and therapies that may help.
Risk Factors for Alzheimer’s
![]() Risk factors for Alzheimer’s include a history of traumatic brain injury or depression. Cardiovascular risk factors, such as high cholesterol, elevated blood pressure, diabetes, and smoking, are also associated with a higher risk of onset and course of Alzheimer’s.
Risk factors for Alzheimer’s include a history of traumatic brain injury or depression. Cardiovascular risk factors, such as high cholesterol, elevated blood pressure, diabetes, and smoking, are also associated with a higher risk of onset and course of Alzheimer’s.
Alzheimer’s Prevention
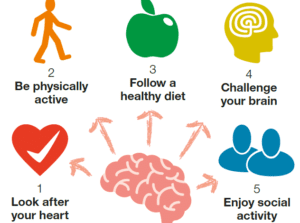
Researchers do not yet know how to prevent all forms of dementia. Most research studies show associations between certain lifestyle factors and Alzheimer’s, but this does not necessarily mean that the factors cause a reduction in risk for Alzheimer’s.
 Specifically…
Specifically…
(a) engaging in physical exercise,
(b) maintaining regular social interaction, and
(c) engaging in mentally-challenging activities (like learning a new language in adulthood, learning an instrument, or playing challenging chess games)
… are associated with reduced age of onset and reduced risk of developing Alzheimer’s.
At this point in time, there are no medications, foods, or vitamins that have been shown conclusively to reduce the risk of progressive dementia, like Alzheimer’s disease. People who maintain a healthy, Japanese, or Mediterranean diet do have a reduced risk of dementia. This is typically attributed to the cardiovascular benefits of such diets.


How is Alzheimer’s Diagnosed?
A diagnosis of Alzheimer’s is made based on:
- clinical interviews with the person and their family members,
- neuropsychological testing (tests of thinking skills), and
- neuroimaging (brain MRIs or CT scans).
Early Detection of Alzheimer’s Disease
Neuropsychological testing of things like memory, word finding, and problems solving can reveal early subtle signs of Alzheimer’s Disease before a person’s activities of daily living are impaired.
When a person’s memory functioning is noticeably worse than their peers on testing, but they are still able to function independently in their lives, this is referred to as Mild Cognitive Impairment (MCI).
What are Common Signs of Alzheimer’s?
The Most Common Early Signs of Alzheimer’s Disease:
- Problems remembering new information
- Difficulty remembering recent events
- Word finding difficulties
- Reduced ability to express yourself with words
Later Signs of Alzheimer’s Disease:
- Worsening memory problems – may have difficulty recognizing familiar faces of family members; may have difficulty remembering key events from the distant past
- Speech difficulties due to inability to remember specific words
- Word substitutions (due to word finding difficulties)
- Problems with reading comprehension or writing skills
- Worsening motor coordination (bumping into things more often, dropping cutlery frequently, difficulty doing up buttons of a shirt, for example) – This can lead to an increased risk for falls
- Increased irritability or frequent crying; depression
- Resistance or fighting against caregivers
- “Sundowning” – this refers to a tendency to become more agitated or confused as the day progresses into late afternoon or evening
- Individuals often lose insight into their limitations or their disease – they may argue that there is no need for help going to the washroom, despite having forgotten how to take care of themselves
- Urinary incontinence (inability to hold one’s urine or get to the bathroom on time)
Treatments for Alzheimer’s
Medications can help improve symptoms of some symptoms of Alzheimer’s but cannot always stop the disease from occurring or eventually progressing. However, there are many treatments that can help support the person and their family in coping and adapting to maintain the best quality of life possible.
Medications can help improve symptoms of Alzheimer’s disease but cannot stop the disease from occurring or eventually progressing.
Psychotherapy may help people in the early stages of Alzheimer’s disease adapt and make preparations for the progression of the illness. Psychotherapy can also help family members cope and prepare for supports to be put in place for their loved ones.
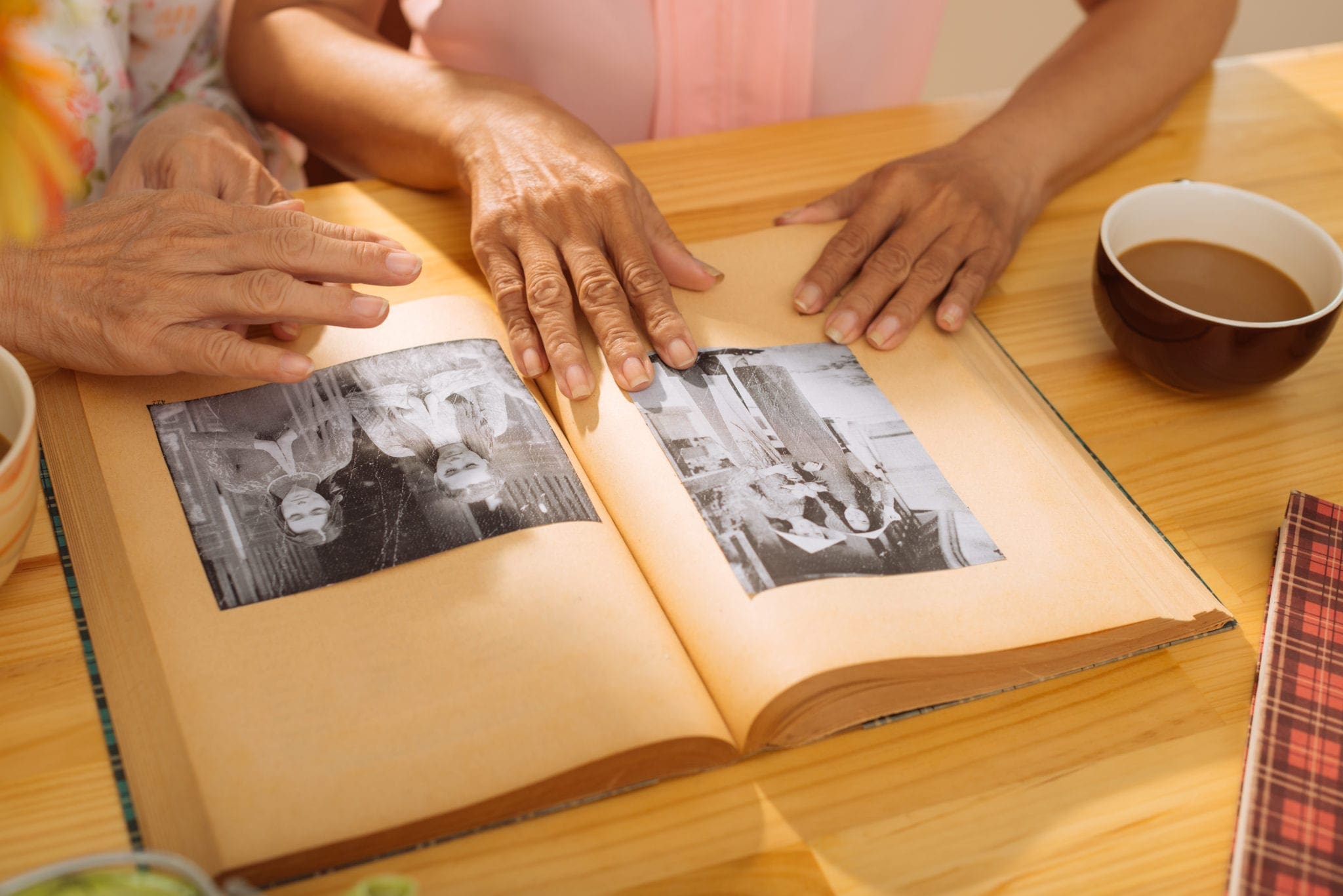
Sometimes “reminiscence therapy” is used in cases of Alzheimer’s disease. Reminiscence therapy allows the person with Alzheimer’s disease re-visit aspects of their life story through reviewing stories, photographs, music, sound recordings, or other familiar reminders of their past.
Sometimes supported recreational activities, like doing art, interacting with service animals, or engaging in gentle exercise routines can provide a sense of life engagement or structure for a person dealing with Alzheimer’s disease. While therapies cannot stop the progression of Alzheimer’s disease, therapies may help bring a sense of meaning to the process.
Help for Caregivers
A person with Alzheimer’s disease requires increasing levels of care-giving over the course of the disease. Without supports, caregivers are at increased risk for depression, anxiety, sleep difficulties, and isolation.
It is important to remember that “The caregiver needs care too!”
Caregivers’ mental health can be benefited by engagement in support groups for caregivers or individual counselling aimed at improving coping strategies.




